In the relentless pursuit of early lung cancer detection, scientists have turned to an unlikely yet promising diagnostic medium: human breath. Recent breakthroughs in nanotechnology have paved the way for highly sensitive sensor arrays capable of detecting volatile organic compounds (VOCs) associated with malignant tumors at their earliest stages. This non-invasive approach could revolutionize how we screen for one of the world's deadliest cancers.
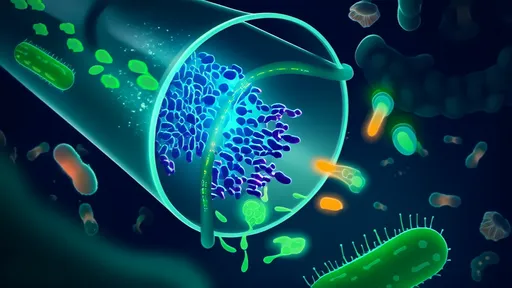
The concept hinges on the fact that cancerous cells produce distinct metabolic byproducts that differ from healthy tissue. These biochemical fingerprints become airborne through respiration, creating unique VOC profiles that nanosensors can theoretically identify. Where traditional methods like CT scans require radiation exposure and often detect cancers at later stages, breath analysis offers a radiation-free alternative with potential for much earlier intervention.
How Nanosensor Arrays Work
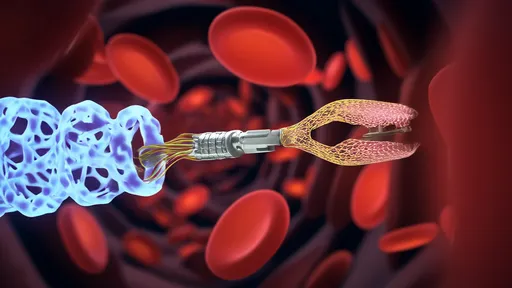
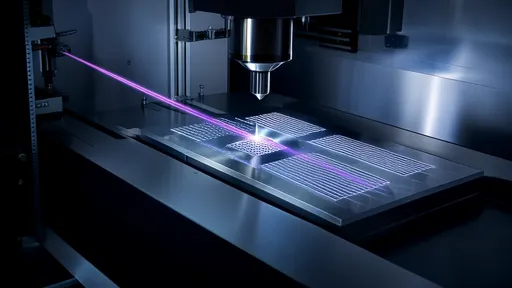
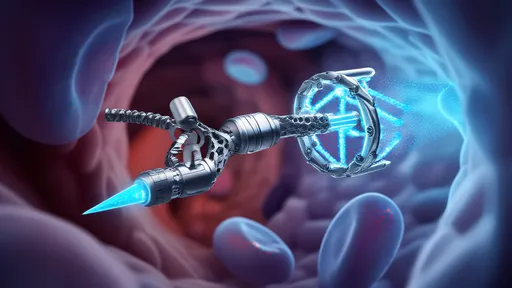
At the heart of this technology lie engineered nanomaterials with extraordinary sensitivity to specific molecular structures. Gold nanoparticles, carbon nanotubes, and quantum dots form the building blocks of these detection systems. When patients exhale into the device, VOCs interact with the sensor surfaces, causing measurable changes in electrical resistance, optical properties, or mass that sophisticated algorithms then decode.
What makes these arrays particularly powerful is their ability to detect patterns across dozens of biomarkers simultaneously. Unlike single-molecule tests that might miss early disease, the multivariate approach accounts for the complex biochemistry of developing tumors. Recent prototypes have demonstrated accuracy rates comparable to imaging techniques for certain cancer types, all while using samples collected through simple breathing maneuvers.
Clinical Validation and Challenges
Several research institutions have published compelling data from trials involving thousands of participants. The Maastricht University Medical Center reported 85% sensitivity in distinguishing early-stage lung cancer from benign nodules using a nanowire sensor platform. Meanwhile, teams at MIT have developed colorimetric sensor arrays that change hue when exposed to cancer signatures, creating visual readouts that don't require complex instrumentation.
However, significant hurdles remain before widespread clinical adoption. Breath contains over 3,000 different VOCs at minute concentrations, and factors like diet, medications, and environmental exposures can complicate readings. Standardizing collection protocols has proven particularly challenging—how patients breathe (tidal volume versus forced exhalation) dramatically affects results. Researchers are working to establish universal sampling methods and control for confounding variables through advanced machine learning techniques.
The Road Ahead
Industry observers predict breath-based screening could enter mainstream medicine within the next decade. Several startups have already commercialized preliminary versions for research use, with designs ranging from desktop analyzers to smartphone-connected portable units. As the technology matures, we may see these devices deployed in primary care offices, pharmacies, and even homes for high-risk populations like long-term smokers.
Perhaps most exciting is the potential to democratize early detection globally. Unlike CT scanners requiring multimillion-dollar investments and specialized operators, breath analyzers could bring affordable cancer screening to resource-limited regions. This aligns perfectly with the World Health Organization's push for equitable access to diagnostic tools that can meaningfully impact survival rates.
The coming years will prove critical as larger longitudinal studies validate these technologies against gold-standard diagnostics. While nanosensor arrays won't replace all existing methods, they may soon give clinicians an invaluable new weapon in the fight against late-stage cancer diagnoses—one breath at a time.

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025